Understanding Eczema: Types, Triggers & Symptoms You Should Know

Eczema is one of the most common skin conditions that affects babies, children, teenagers, and adults. According to the National Eczema Association, this chronic skin condition affects around 10 to 20% children and 2 to 10% adults worldwide.
While in the USA, more than 31.6 million people have some type of eczema. If you or your loved one is experiencing eczema for the first time and you don’t know much about it, then this blog is for you.
It will help you learn everything from what eczema is, what causes it, common triggers, eczema types, to how to manage it effectively.
What is Eczema?
Eczema is an inflammatory skin condition that causes dry, red, itchy, irritated skin. However, the truth is, eczema isn’t just one condition; in fact, there are different types of eczema that cause similar symptoms.
When you are experiencing eczema, the skin’s natural barrier becomes weak, making it hard for the skin to retain moisture and easier for the outside irritants and allergens to penetrate the skin.
This is why people with eczema have extra-sensitive skin. Even though eczema is more common among children, anyone can experience it at any age. It is a chronic condition, which means it either resolves or becomes a lifelong issue and appears again and again in the form of flare-ups.
According to the National Eczema Association, an eczema flare-up is the duration when the symptoms become intense, and remission is the period when the symptoms soothe down.
Eczema Symptoms
We know that itching is one of the most common symptoms of eczema; however, the itching may vary from person to person depending on the severity of the condition. For some, it is just a mild itch, while for others, it may disrupt their sleep and quality of life.
Along with the itch, some other common eczema symptoms that you may notice are:
- Dry skin
- Flaky, cracked skin
- Inflammation
- Redness
- Scaly or rough texture of skin
- Rashes that may swell
- Small, raised bumps and blisters
- Oozing or crusting skin
- Leathery patches on skin
- Skin discoloration
The symptoms may vary from person to person; some may experience just one or two during a flare-up, while others may experience more than that. Eczema can appear anywhere on the body; however, some of the most affected areas are:
- Hands
- Feet
- Elbows
- Knees
- Face
- Ankles
- Neck
- Upper chest
- Round the ears
- Skin folds
Apart from these, eczema, even though it is less common, can also affect sensitive areas of the body, like nipples, breasts, genitals, and the groin area.
What Does Eczema Look Like?
Now you know what symptoms eczema can cause on your skin, but you might still be wondering what it looks like. Eczema usually appears differently on everyone, especially depending on your skin color and the type of eczema you are experiencing.
For instance, the redness may appear reddish or pinkish in people with lighter skin tones, while in people with darker skin tones, it may appear as brown, purple, gray, or darker than the skin tone.
Also, skin thickening and dark patches around the eyes are more common in people with dark skin. It is also essential to understand that eczema can change in appearance from time to time, depending on the stage of the condition.
What Causes Eczema?
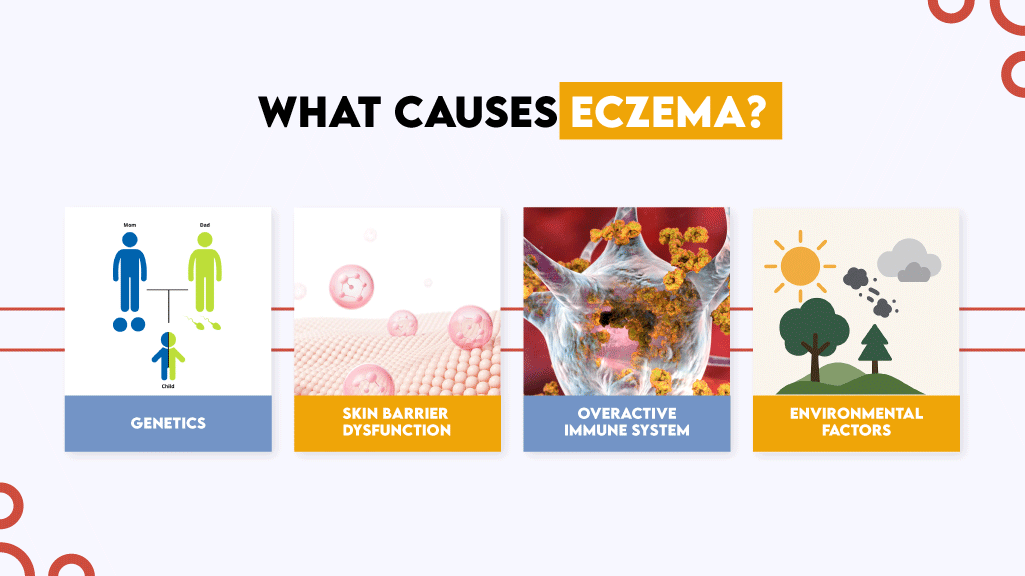
Most people think that dry skin is the cause of eczema; however, this is not the case. The exact cause of eczema is still not known; however, it is believed to be caused by a combination of factors such as:
Genetics
Genetics plays a primary role in developing eczema. People who have a family history of eczema, atopic dermatitis, hay fever, asthma, and allergies are more prone to developing eczema.
According to the National Eczema Association, if both of your parents have eczema, then you are 50% more likely to experience it at some point in your life. This is because some people carry a gene mutation that weakens the skin’s natural barrier and makes one more prone to eczema.
Skin Barrier Dysfunction
The gene that is responsible for developing a strong skin barrier is the filaggrin gene. When there is a mutation or variation in that gene, the barrier becomes weak, due to which the outside irritants and allergens can penetrate the skin and cause inflammation.
Additionally, the skin is unable to retain moisture properly, resulting in dryness, itching, and irritation caused by eczema.
Overactive Immune System
Some researchers also believe that eczema can be triggered due to an overactive immune system. When you have an overactive immune system, it can react to even minor irritants that are usually not harmful to your skin or body.
And as a result, the immune system triggers inflammation in the body, which appears in the form of redness, rashes, and irritation on the skin.
Environmental Factors
There are various factors around us in our environment that can cause a reaction on eczema-prone sensitive skin and lead to an eczema flare-up. Let’s learn a little more about these triggers.
What Triggers Eczema?
The list of eczema triggers is very long; they can either be something from the environment or even your emotional well-being. However, below we have listed some of the most common ones:
- Dry skin
- Stress
- Skin infections
Environmental Irritants
- Cold, dry air
- Tobacco smoke
- Pollution
- Pollen
- Mold
- Dust mites
- Weather conditions
- Extreme heat and sweating
Allergens
- Pet dander
- Insect bites
- Pollen
- Poison ivy
- Metals (nickel, copper, gold, and chlorium)
- Certain foods
Irritating Material
- Rough fabrics such as wool
- Latex
- Harsh chemicals in skin care products
- Fragrances
- Chemicals in cleaning products
The triggers may vary from person to person. These triggers can either cause an eczema flare-up or make the existing symptoms worse; this is why identifying and avoiding them is essential to managing eczema.
Types of Eczema
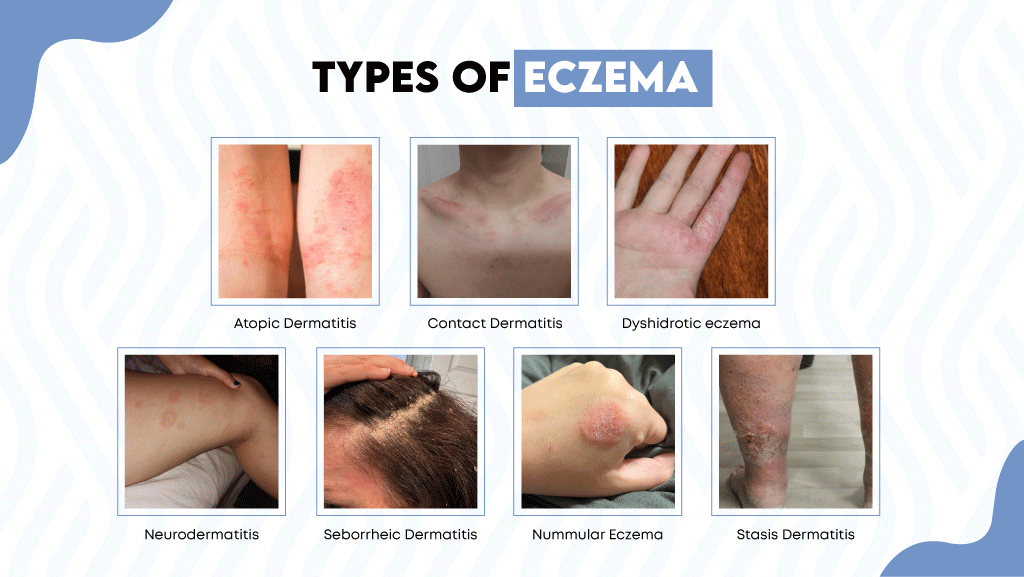
Most people don’t know, but there are 7 different types of eczema. The symptoms and treatment for each type of eczema may vary a little; however, almost all of these cause itching and irritation on the skin.
Here are the types of eczema with pictures to help you identify them:
1. Atopic Dermatitis
Atopic dermatitis is the most common type of eczema. It is more common in childhood and infancy; children under the age of 6 are more likely to experience it for the first time in their lives.
However, this does not mean that it can not appear for the first time in adulthood; when adults experience it, it is usually known as adult-onset eczema. People who have a family history of atopic dermatitis are more likely to experience it. Also, it is believed to be caused by a compromised skin barrier and environmental triggers.
Atopic Dermatitis Symptoms
- Intense itching
- Dry patches on skin
- Skin discoloration
- Cracked or scaly skin
Treatment and Management
Although there is no permanent cure for atopic dermatitis, consistent skincare can keep symptoms under control and help prevent flare-ups. Dermatologists typically recommend:
- Gentle cleansing: Use a mild, fragrance-free eczema body wash that removes impurities without stripping natural oils.
- Moisturizing frequently: Apply a dermatologist-approved eczema cream several times a day to hydrate and strengthen the skin barrier.
- Avoiding triggers: Minimize exposure to irritants, allergens, and extreme temperatures that can aggravate dryness and itching.
- Professional care for flares: For moderate to severe symptoms, dermatologists may prescribe topical anti-inflammatory creams or other targeted treatments to calm irritation.
Consistent use of gentle cleansers and moisturizers is the foundation of long-term atopic dermatitis care. They help reduce dryness, restore comfort, and support the skin’s natural barrier.
2. Contact Dermatitis
Contact dermatitis occurs when your skin comes in contact with something that irritates or causes an allergic reaction. Even though it can appear anywhere on the body, it is more common on the body parts that are often exposed to irritants, such as the face, hands, and feet.
There are two further types of contact dermatitis
Irritant contact dermatitis
It is when your skin comes in contact with something that irritates your skin, such as alcohol, soap, detergents, fragrances, and cleaning chemicals. It causes a direct reaction on the skin and usually does not involve the immune system.
Allergic dermatitis contact
It is when your skin comes in contact with a certain allergen that your immune system considers a threat and causes an allergic reaction on the skin. The symptoms usually start appearing 12 to 48 hours after coming in contact with the allergen.
Contact Dermatitis Symptoms
- Itchy skin
- Red rashes
- A burning or stinging sensation
- Thick, leathery skin
- Blisters and hives
Treatment and Management
While contact dermatitis often improves once the trigger is removed, proper skin care can help soothe irritation and restore the skin barrier:
- Identify and avoid irritants: Try to determine what caused the reaction—common triggers include fragrances, cleaning products, and certain metals like nickel.
- Cleanse gently: Wash the affected area with a mild, fragrance-free cleanser such as the Dermal Defense Sensitive Skin Body Wash to remove irritants without stripping moisture.
- Moisturize frequently: Apply a rich, dermatologist-approved moisturizer like the Dermal Defense Eczema Moisturizing Cream to help hydrate the skin and support recovery.
- Protect your skin: Use gloves or protective clothing when handling cleaning agents, detergents, or other irritants.
- Soothe flare-ups: Cool compresses can temporarily relieve itching and inflammation.
- Consult a dermatologist: For severe, persistent, or infected cases, a healthcare professional may prescribe short-term topical corticosteroids or other targeted treatments.
- With consistent care and avoidance of known irritants, most cases of contact dermatitis can be effectively managed, helping the skin return to its normal, healthy state.
3. Dyshidrotic eczema
Dyshidrotic eczema, also known as pompholyx eczema, causes painful, itchy blisters on the hands, fingers, feet, and toes. This type of eczema is more common among adults over 40.
These blisters usually last for a few weeks or may occur repeatedly from time to time. Some of the triggers that make the condition worse are sweat, heat, and stress.
Dyshidrotic Eczema Symptoms
- Fluid-filled blisters
- Itching
- Burning or stinging sensation
- Peeling and flaking skin
Treatment and Management
Managing dyshidrotic eczema focuses on soothing irritation, protecting the skin barrier, and preventing flare-ups. While severe cases may require prescription creams or other medications, consistent at-home care plays a major role:
- Cleanse gently: Use a mild, fragrance-free cleanser such as the Dermal Defense Sensitive Skin Body Wash to remove sweat, bacteria, and irritants without drying out the skin.
- Moisturize often: Keep the skin hydrated with a rich, eczema-friendly moisturizer like the Dermal Defense Eczema Moisturizing Cream. Reapply after washing hands or bathing to maintain the skin barrier.
- Avoid triggers: Limit contact with harsh cleaning products, detergents, and prolonged water exposure. Wear protective gloves for household chores, especially when washing dishes or cleaning.
- Soothe discomfort: Apply cool compresses to reduce itching and inflammation. Avoid scratching, as this can worsen irritation or cause infection.
- Manage stress and sweating: Stress reduction, staying cool, and using breathable gloves or socks can help reduce flare frequency.
- Consult a dermatologist: For persistent or severe cases, a dermatologist may recommend prescription topical corticosteroids, non-steroidal anti-inflammatories, or light therapy (phototherapy).
With consistent care, hydration, and trigger awareness, most people can reduce the frequency and intensity of dyshidrotic eczema flare-ups and maintain calmer, healthier skin.
4. Neurodermatitis
Neurodermatitis, also known as Lichen Simplex Chronicus, usually starts as patches of skin that cause intense itching. The more you itch your skin, the worse it gets. Neurodermatitis usually affects one or two areas of the body and is often linked to or becomes worse due to stress and anxiety.
Neurodermatitis symptoms
- Thick scaly patches
- Intense itching
- Cracked, raw skin
- Skin discoloration
Treatment and Management
Managing neurodermatitis focuses on breaking the itch-scratch cycle, restoring moisture to the skin, and addressing underlying triggers such as stress or anxiety.
- Moisturize regularly: Apply a rich, fragrance-free moisturizer such as the Dermal Defense Eczema Moisturizing Cream several times a day to soothe dryness and strengthen the skin barrier.
- Cleanse gently: Use a mild, non-irritating cleanser like the Dermal Defense Sensitive Skin Body Wash to keep skin clean without causing additional irritation.
- Avoid scratching: Cover affected areas with soft clothing or bandages if needed, and keep nails trimmed to prevent skin damage.
- Relieve itching: Applying cool compresses or using over-the-counter anti-itch creams (as advised by a healthcare professional) can help reduce discomfort.
- Manage stress: Since stress is a key trigger, incorporating relaxation techniques such as meditation, yoga, or regular exercise can help reduce flare-ups.
- Consult a dermatologist: For persistent or severe cases, a doctor may prescribe topical corticosteroids, non-steroidal anti-inflammatories, or other medications to calm inflammation and relieve itching.
With consistent moisturization, gentle cleansing, and stress management, most individuals can greatly reduce flare intensity and prevent recurrence of neurodermatitis.
5. Seborrheic Dermatitis
Seborrheic dermatitis, also known as scalp eczema, or cradle cap when it appears in babies, is a skin condition that causes thick, greasy, yellow or white scales on the scalp, beard, and eyebrows. Along with the scaling and flaking, it also causes redness and inflammation on the skin, especially behind the ears, around the nose, and in the skin folds.
The causes of seborrheic dermatitis are a little different from the rest of the types of eczema. It is believed to be caused by a combination of factors such as overactive sebaceous glands, the presence of excess sebum, overgrowth of malassezia yeast on the skin, and skin sensitivity towards oleic acid.
Seborrheic Dermatitis Symptoms
- Yellow or white flakes and scales
- Inflamamtion
- Redness on the skin
- Thick, greasy scales
Treatment and Management
Because seborrheic dermatitis is a chronic, relapsing condition, treatment focuses on controlling yeast growth, reducing flaking, and calming inflammation rather than curing it completely.
- Cleanse regularly: Use a gentle, medicated cleanser or shampoo specifically formulated for seborrheic dermatitis at least 2–3 times per week to help reduce yeast buildup and excess oil.
- A dermatologist-recommended option is the Facial Fortress 3-in-1 Medicated Wash by Dr. Eddie, which contains Zinc Pyrithione, an FDA-approved active ingredient proven to help relieve dandruff and seborrheic dermatitis on the scalp, face, and beard.
- Moisturize after cleansing: Apply a light, non-comedogenic moisturizer such as the Dermal Defense Eczema Moisturizing Cream to soothe dryness and support the skin barrier after washing.
- Avoid harsh products: Fragrance, alcohol-based toners, and aggressive exfoliants can worsen irritation. Stick to fragrance-free, gentle skincare.
- Manage triggers: Stress, cold weather, and lack of sleep can all trigger flare-ups. Practice regular stress management and maintain a consistent skincare routine.
- Consult a dermatologist: For severe or persistent cases, your doctor may recommend short-term use of prescription antifungal or anti-inflammatory treatments to control symptoms more effectively.
With regular cleansing, proper moisturization, and consistent care, most people can significantly reduce the scaling, itching, and redness caused by seborrheic dermatitis and maintain healthy-looking skin.
6. Nummular Eczema
Nummular eczema, also known as discoid eczema, usually appears as round, coin-shaped patches that can appear anywhere on the body. Even though anyone can experience it, it is more common among young adults and older children.
These patches can be very dry, itchy, and flaky, which is why this eczema is often confused with another common skin condition known as ringworm.
Symptoms of Nummular Eczema
- Round patches of inflamed skin
- Tiny bumps and blisters
- The bumps may ooze and crust
- Scaly patches of skin
Treatment and Management
Managing nummular eczema focuses on rebuilding the skin barrier, locking in moisture, and preventing flare-ups.
- Bathe gently: Take short baths in lukewarm (not hot) water to avoid stripping away natural oils. Add a mild, fragrance-free cleanser such as the Dermal Defense Sensitive Skin Body Wash to remove impurities without drying the skin.
- Moisturize immediately after bathing: Within three minutes of stepping out of the bath, apply a rich, emollient moisturizer such as the Dermal Defense Eczema Moisturizing Cream to trap moisture and strengthen the skin barrier.
- Use a humidifier: Keep indoor air moist, especially during cold or dry seasons, to help prevent skin dehydration.
- Avoid irritants: Stay away from harsh soaps, detergents, and heavily fragranced products that can trigger itching or flare-ups.
- Wear soft, breathable fabrics: Cotton or bamboo clothing helps minimize irritation compared to wool or synthetic fibers.
- Consult a dermatologist: For more severe or persistent cases, your doctor may recommend medicated options such as topical corticosteroids, calcineurin inhibitors (like tacrolimus), or coal tar–based creams to reduce inflammation and itching.
Consistent moisturization and gentle daily care are key to controlling nummular eczema. With the right skincare routine and avoidance of triggers, symptoms can be greatly reduced, and flare-ups become less frequent over time.
7. Stasis Dermatitis
Stasis dermatitis usually develops due to poor blood circulation, especially in the lower legs. This is why it is more common among adults above the age of 50. When your veins struggle to send blood back to the heart, this condition is known as varicose veins.
Due to this, the veins start leaking fluid into the skin, which causes swelling, redness, and inflammation.
Stasis Dermatitis Symptoms
- Swelling in the ankles and legs
- Skin discoloration
- Itching
- Scaly, dry skin
- Open sores and ulcers in severe cases
Treatment and Management
While there is no permanent cure for stasis dermatitis, proper care can significantly reduce symptoms, prevent complications, and improve circulation. The main goals are to improve blood flow, reduce swelling, and protect the skin barrier.
- Keep the skin moisturized: Apply a rich, fragrance-free cream such as the Dermal Defense Eczema Moisturizing Cream daily to soothe dryness, reduce flaking, and strengthen the skin’s protective barrier.
- Cleanse gently: Wash with a mild, pH-balanced cleanser like the Dermal Defense Sensitive Skin Body Wash to keep skin clean without further irritation or dehydration.
- Support circulation: Engage in regular, low-impact exercise such as walking, which helps pump blood back toward the heart.
- Elevate your legs: Raise your legs above heart level for 15–20 minutes several times a day to help reduce swelling.
- Wear compression garments: Use compression socks or stockings if recommended by your doctor to support vein function and reduce fluid buildup.
- Avoid prolonged standing or sitting: Move around frequently to encourage healthy blood flow.
- Maintain a healthy weight: Excess body weight increases pressure on the veins, which can worsen the condition.
- Consult a healthcare professional: For severe inflammation, ulcers, or signs of infection, a doctor may prescribe topical corticosteroids, antibiotics, or specialized wound care.
Consistent moisturization, movement, and compression therapy can greatly improve comfort and skin health in people with stasis dermatitis while reducing the risk of flare-ups or ulcer formation.
Eczema Treatment

While there is no permanent cure for eczema, it can be effectively managed through consistent skincare and trigger avoidance. Each type of eczema may require slightly different care, but the foundation of every eczema management plan is the same: gentle cleansing, daily moisturization, and protecting the skin barrier.
Step 1: Gentle Cleansing
Use a soap-free, fragrance-free cleanser designed for sensitive or eczema-prone skin. Cleansing once daily—twice if you’re active or exposed to sweat and pollutants—helps remove impurities without stripping natural oils.
A product like the Dermal Defense Sensitive Skin Body Wash can be a good choice. It combines botanical extracts such as licorice root, oat, apple, and aloe vera, along with provitamin B5, to calm irritation while supporting skin hydration.
Step 2: Daily Moisturizing
Immediately after bathing, apply a hypoallergenic, fragrance-free moisturizer to seal in moisture and strengthen the skin’s natural barrier. Look for a formula rich in emollients and humectants such as petrolatum and glycerin.
The Dermal Defense Eczema Moisturizing Cream contains snow-white petrolatum, glycerin, and licorice extract, which help soothe dryness, relieve itching, and restore the barrier function of eczema-prone skin.
Step 3: Avoid Triggers and Support Skin Health
Identify and minimize contact with known irritants such as harsh soaps, detergents, and fragrances. Maintain a balanced diet, manage stress, and use a humidifier during dry weather to prevent flare-ups.
Key Takeaways
- Eczema is a chronic skin condition that causes red, itchy, dry, irritated rashes and patches of skin.
- Eczema is not just one condition; it has seven different types: atopic dermatitis, contact dermatitis, neurodermatitis, seborrheic dermatitis, nummular eczema, stasis dermatitis, and dyshidrotic eczema.
- The treatment for each type may vary a little, but following an eczema skincare routine that includes cleansing the skin and moisturizing it is essential for every type.
FAQs
- Does eczema go away on its own?
In some cases, eczema can go away on its own and resolve properly, while in most cases it requires proper care and treatment to prevent the condition from getting worse.
- What is the main cause of eczema?
There is no exact cause for eczema; in fact, it is believed to be caused by a combination of factors such as
- Genetics
- Skin barrier dysfunction
- Overactive immune system
- Environmental triggers
- Can eczema spread by scratching?
Eczema usually does not spread from scratching; however, if you scratch your eczema, it triggers a never-ending itch-scratch cycle that can further worsen your condition and, in some cases, lead to complications like skin infections.
- What is the best treatment for eczema?
There is no permanent cure for eczema; however, following a proper skin care routine that includes cleansing the skin daily with an eczema cleanser and keeping it moisturized with the help of an eczema cream, and avoiding the triggers is the best way to soothe the itching and irritation caused by eczema.
- How many types of eczema are there?
There are seven different types of eczema
- Atopic dermatitis
- Contact dermatitis
- Neurodermatitis
- Seborrheic dermatitis
- Nummular eczema
- Stasis dermatitis
- Dyshidrotic eczema
- How often should I shower with eczema?
It is usually prescribed by doctors to take a bath at least once daily if you have eczema. However, make sure the water you are using is lukewarm, and the body wash you are using is specially formulated for eczema-prone, sensitive skin and is fragrance-free, paraben-free, sulfate-free, dye-free, and alcohol-free.
- Eczema and the Immune System: Is It Autoimmune or Immune-Mediated? - February 18, 2026
- Eczema on Black Skin and Other Skin Tones: How It Looks, Symptoms, and Diagnosis - February 18, 2026
- The Link Between Eczema and Allergies: Triggers, Atopic March, and Managing Flare-Ups - February 18, 2026