Psoriasis vs Eczema: How to Tell the Difference
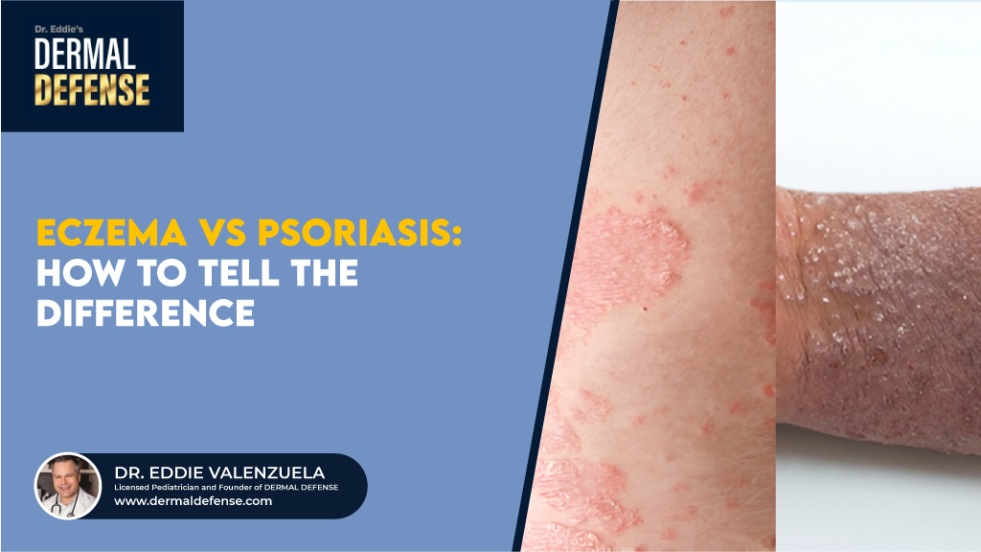
Psoriasis vs Eczema: Which condition are you dealing with? It becomes quite difficult to identify each condition because both have some common symptoms. Obviously, you can consult a professional for a proper diagnosis. But in this article, we aim to differentiate between eczema and psoriasis so you can diagnose them yourself. Plus, we have also explained their treatment strategies and management tips for both.
Psoriasis vs Eczema: Common Symptoms
Due to commonality in symptoms, they are often considered the same. However, they are entirely different conditions. Some symptoms are common in eczema and psoriasis.
- Inflammation
- Redness
- Itching
- Burning sensation
- Rash
- Dry and cracked skin
- Scaly patches
- Discoloration
Even if there are several similar symptoms, there is still space for the identification of each condition. Before we move on to psoriasis vs eczema differences, let’s first elaborate on each condition.
What Is Eczema?
Eczema is a long-lasting skin condition that results in scaly patches, rash, and discoloration on the skin. It usually develops in childhood, and the symptoms can appear even in older adults. However, it is more common in children under 5.
This skin disease requires treatment, as negligence in its management could lead to severe symptoms. Severe eczema can also lead to oozing blisters and even infection on the skin.
There is no known cause of eczema, but it is believed to be caused by a combination of genetic and environmental factors. Harsh environments, irritants, infection, and stress can exacerbate eczema.
Currently, there is no permanent cure for this condition. There are some ways to soothe its symptoms, but the condition can recur.
Common Types of Eczema
There are certain types that are more recurring or commonly seen:
- Atopic Dermatitis: The most common one. This type is caused by internal body factors (weak skin barrier, genetics, and allergic reactions). It makes the skin dry, itchy, and irritated.
- Contact Dermatitis: As its name suggests, it appears when irritants like soaps, detergents, or metals trigger the skin. When your skin comes into contact with these allergens, it will become dry, itchy, and irritated, and will develop a rash.
- Dyshidrotic Eczema: This type of eczema leads to small, itchy blisters on the hands and feet. It is triggered by moisture and allergens.
- Nummular Eczema: This results in circular, coin-shaped patches that are dry and itchy. It often looks like a ringworm, but the difference is that nummular eczema patches tend to be uniformly dry. This is a tricky distinction to make.
- Seborrheic Dermatitis: Often known as a severe case of dandruff in adults and cradle cap in children. This condition leads to scaly and greasy patches on the skin along with irritation, redness, and flakiness. The skin is usually oily.
Key Symptoms of Eczema
These are some common symptoms of eczema, regardless of age and gender:
- Inflammation
- Redness
- Rashes on the skin
- Discolored patches on the skin
- Scaly patches
- Itching
- Burning sensation
These are general symptoms in mild to normal conditions. However, eczema on black skin is difficult to diagnose and shows slightly different symptoms. The rash will look purple, and symptoms will be less visible. Late diagnosis can also lead to a more severe condition.
What is Psoriasis?
Psoriasis is a chronic autoimmune skin condition in which the body’s immune system mistakenly speeds up the life cycle of skin cells. Instead of renewing over several weeks, skin cells regenerate and shed in just a few days. This rapid turnover causes a buildup of thick, dry, scaly patches known as plaques that often appear red, pink, or silver-white in color.
These plaques may itch, burn, crack, or become painful, and can appear on the scalp, elbows, knees, lower back, or other areas of the body. While psoriasis is not contagious, it can be highly visible and emotionally distressing. Many people struggle with self-esteem issues, anxiety, or depression due to the appearance of their skin. Some people even develop suicidal thoughts.
Unlike temporary rashes or eczema flare-ups, psoriasis tends to persist or recur throughout life, with symptoms that can worsen during certain triggers such as stress, cold weather, infections, or medications.
Psoriasis affects men and women of all ages and ethnicities, though it is most commonly diagnosed in adults. While there is no permanent cure, effective treatments and proper skincare can help manage flare-ups, reduce inflammation, and improve the overall appearance and comfort of the skin.
Common Types of Psoriasis
Here are some common types of psoriasis.
- Plaque Psoriasis: Is the most common type that leads to thick, scaly patches, often on the elbows, knees, and scalp.
- Guttate Psoriasis: This type leads to small, drop-shaped spots, often triggered by infections.
- Inverse Psoriasis: It affects skin folds, like under the breasts or the groin area. The skin develops red, inflamed, but smooth patches.
- Pustular Psoriasis: As its name suggests, it leads to pus-filled bumps surrounded by red skin.
- Erythrodermic Psoriasis: This is a rare but severe type of psoriasis. It causes widespread redness and shedding of skin.
Key Symptoms of Psoriasis
The prominent and most common symptoms of psoriasis are:
- Inflammation
- Patches on the skin
- Silvery, red, or pink plaques
- Itching
- Redness
- Pain in the affected area
- Burning sensation
Psoriasis vs Eczema: Key Differences

Even though they have common symptoms, there are some key differences between psoriasis and eczema.
Appearance of Rashes
Eczema and psoriasis can both cause red, scaly patches on the skin, but they look and feel quite different.
In eczema, the rash usually appears dry, rough, and scaly, with areas of redness or irritation. On darker skin tones, eczema may look purple, gray, or ashy brown instead of bright red. The skin often feels itchy, tight, or inflamed, and scratching can lead to oozing or crusting.
In psoriasis, the rash is typically thicker, more raised, and more inflamed. The affected skin forms well-defined plaques covered with silvery-white scales that may appear pink, red, or purplish depending on the person’s skin tone. Psoriasis patches tend to look sharper and more prominent than eczema and often occur on the scalp, elbows, knees, and lower back.
Location on the Body
The location of the rash can help distinguish eczema from psoriasis.
Eczema most often appears in skin folds and creases, such as the elbows, behind the knees, armpits, neck, and around the eyes or mouth. The skin in these areas may become red, dry, and itchy, sometimes cracking or oozing when scratched.
Psoriasis, on the other hand, tends to appear on the outer surfaces of the body, forming thick, raised plaques on areas such as the scalp, elbows, knees, lower back, buttocks, and face. However, both conditions can occur anywhere on the body, including the hands, feet, and trunk.
Itch vs. Pain
Both eczema and psoriasis cause discomfort, but the type of sensation differs.
Eczema causes intense itching that can become unbearable, often leading to scratching and further irritation or skin damage.
Psoriasis usually produces a combination of itching, burning, and stinging pain. The affected areas often feel tight, sore, or inflamed, especially when plaques crack or dry out. In many cases, people describe psoriasis as more painful, while eczema is more itch-dominant.
Flare-Up Triggers
Eczema flare-ups are often triggered by environmental irritants or skin sensitivity. Common eczema triggers include:
- Harsh soaps, detergents, and cleaning chemicals
- Rough fabrics such as wool or synthetic materials
- Hot weather, sweat, or humidity
- Cold, dry air and seasonal changes
- Allergens like dust mites, pollen, and pet dander
Psoriasis flare-ups, in contrast, are linked more to immune and lifestyle factors, such as:
- Emotional stress or anxiety
- Skin injuries (cuts, burns, or even tattoos)
- Infections, particularly strep throat
- Smoking and excessive alcohol consumption
- Certain medications and climate changes
Understanding these triggers can help reduce flare-ups and improve the effectiveness of treatment plans for both conditions.
| Eczema | Psoriasis |
| The rash is red, dry, and scaly. | The rash is very scaly, crusty, and more prominent. |
| It leads to intense itching. | It is more painful and burning. |
| Flare-ups occur due to allergens, harsh chemicals, heat, and specific fabrics. | Flare-ups occur due to medications, smoking, skin injuries, and infections. |
| It often appears in skin folds. | It often appears on the outer skin. |
Which Condition Is More Serious Overall?
While both eczema and psoriasis can greatly affect a person’s quality of life, psoriasis is generally considered more serious.
Eczema causes inflamed, dry, and itchy patches that can lead to discomfort and sleep disruption, but it often improves with consistent skincare and trigger management.
Psoriasis, however, tends to form thicker, more painful plaques that are visibly raised and covered with silvery scales. These plaques not only cause burning, stinging, or soreness, but can also lead to emotional distress, as many people feel self-conscious about their appearance. The visible nature of psoriasis can contribute to social withdrawal, anxiety, and depression.
Beyond the skin, psoriasis is an autoimmune disorder that can affect the entire body. In some people, it can progress to psoriatic arthritis, a condition that causes joint pain, stiffness, and swelling, potentially leading to long-term mobility issues if untreated.
Although eczema flare-ups can be extremely uncomfortable, psoriasis carries a higher overall health risk because of its systemic nature and chronic complications.
Psoriasis vs. Eczema: Symptom Management
Over-the-counter (OTC) treatments are widely available for both psoriasis and eczema. For psoriasis, look for products that contain coal tar or salicylic acid as active ingredients—both help reduce scaling and slow rapid skin cell turnover. Regular use of rich, fragrance-free moisturizers or lotions also helps soften thick plaques and soothe irritation.
For eczema, choose a gentle moisturizer that includes colloidal oatmeal or glycerin to calm inflammation and hydrate the skin. The Eczema Moisturizing Cream by Dermal Defense, developed by Dr. Eddie, meets these criteria—it is designed specifically for sensitive, eczema-prone skin.
When selecting any skincare product, always make sure it is free of harsh chemicals, dyes, and fragrances that can worsen irritation.
Daily Management Tips

1. Moisturizing & Skincare Routines
Both eczema and psoriasis cause dry, scaly, and inflamed skin, which makes daily moisturizing essential. Gently cleanse the affected area to remove dirt and bacteria before applying a soothing moisturizer.
Regular moisturizing helps:
- Prevent flare-ups
- Reduce itching and burning
- Restore the skin barrier
- Calm inflammation
For eczema, the Dermal Defense Eczema Moisturizing Cream pairs best with a sensitive-skin body wash from the same line, offering a complete routine to keep skin hydrated and comfortable.
2. Diet and Lifestyle Choices
Your diet plays an important role in skin health.
For eczema, avoid foods that often trigger inflammation, such as eggs, peanuts, dairy, and certain beans. Focus on a diet rich in green vegetables, fruits, and whole grains.
For psoriasis, a Mediterranean-style diet works best. Include omega-3 fatty acids, olive oil, fatty fish, fruits, and vegetables, and avoid processed foods, high-sugar snacks, and red meat, which can worsen flare-ups.
3. Stress Management
Stress is a major trigger for both eczema and psoriasis. It weakens the immune system and damages the skin barrier, increasing the risk of flare-ups and infections.
To reduce stress and support skin healing:
- Practice yoga or meditation
- Spend time with family and friends
- Exercise regularly
- Maintain a balanced diet
- Get adequate sleep
- Seek therapy or counseling if stress feels overwhelming
A calm mind and consistent routine can greatly improve long-term skin health.
When to See a Dermatologist
Seek professional care if you experience:
- Severe pain, swelling, or oozing blisters
- Signs of infection (odor, pus, or spreading redness)
- Bleeding or cracked skin
- Uncontrollable itching or burning
- Emotional distress related to your skin condition
A board-certified dermatologist can confirm your diagnosis, recommend prescription treatments, and help manage flare-ups safely and effectively.
Living with Psoriasis or Eczema: Final Thoughts
Both psoriasis and eczema can be challenging, but with the right skincare, lifestyle habits, and professional guidance, their symptoms can be managed effectively. Avoid known triggers, keep skin hydrated, and maintain a healthy daily routine to reduce flare-ups and improve comfort.
FAQs About Eczema vs. Psoriasis
Can you have both eczema and psoriasis at the same time?
Yes, although rare, some individuals can experience both conditions simultaneously. This guide helps you understand their differences and choose the right management plan.
Which one is more serious?
In general, psoriasis is more severe because it can cause systemic inflammation and joint complications such as psoriatic arthritis, and it often requires long-term medical treatment.
Do both conditions run in families?
Yes. Genetics play a role in both eczema and psoriasis, though psoriasis tends to have a stronger hereditary link.
Is either condition contagious?
No. Neither eczema nor psoriasis is contagious. You cannot catch them through physical contact. However, both can spread to other parts of your own body during flare-ups.
- Eczema and Mental Health: How It Affects Anxiety & Depression - January 29, 2026
- Eczema and Genetics: Is It Hereditary? - January 29, 2026
- Is Eczema Contagious? Debunking Myths - January 27, 2026