Eczema and Genetics: Is It Hereditary?

Doctor Answer: Is Eczema Genetic?
Yes. Eczema has a strong genetic component, but it is not caused by genes alone.
Many people inherit a genetic tendency that affects the skin barrier or immune response, which increases the risk of eczema. Environmental triggers often determine when and how symptoms appear.
If you’re a parent living with eczema, you may have wondered: Is eczema hereditary? Can I pass it on to my children? The short answer is yes.
But what’s the science behind eczema running in families? In this blog, we’ll explore the link between eczema and genetics and some of the most effective ways to manage eczema for you and your little ones.
What is Eczema?
Eczema, also known as atopic dermatitis, is an inflammatory chronic skin condition that leads to red rashes that may flare up and subside over time. Eczema is more common among children below the age of 5 and usually resolves by adolescence.
But some individuals may continue to experience flare-ups even in adulthood. When you experience eczema, the skin’s protective barrier becomes weak due to which makes it unable to retain moisture properly and protect the skin against outside irritants.
Some common eczema symptoms that you may experience during a flare-up are:
- Dry skin
- Rough, scaly patches
- Redness
- Inflamed skin
- Intense itching
- Skin lichenification
The symptoms may vary from person to person, and the redness associated with it often appears as red or pink in lighter skin tones and gray, brown, or purple on darker skin tones.
The Connection Between Eczema and Genetics
The answer to “Is eczema genetic?” is a little complicated. According to research, genetic predisposition plays an essential role in developing eczema. However, you can say it is partially genetic and partially triggered by environmental factors.
Now you might be wondering how genetics can cause eczema. Genetics can significantly impact how the skin barrier and immune system function.
- Genetics Affecting the Skin Barrier
There is a protein present in our body known as filaggrin that helps strengthen the skin’s natural barrier. Mutations in genes such as FLG (filaggrin) and other skin-barrier–related genes can impair the skin’s ability to retain moisture and protect against irritants.
This makes the skin more vulnerable to irritation, moisture loss, and secondary skin infections, which leads to dry, itchy, irritated skin.
- Genetics Affecting the Immune System
Genetics can have an impact on the body’s immune system. A mutation in the IL-4 and IL-13 genes can lead to an overactive immune system, due to which the skin may overreact towards certain allergens that are not actually harmful. IL-31, a cytokine involved in itch signaling, can contribute to intense itching and inflammation in people with eczema.
Is Eczema Hereditary?
Yes, eczema can be hereditary; it often runs in families. According to the Allergy and Asthma Network, approximately 70% of people with eczema have a family history of the condition. Also, people who have a family history of asthma, hay fever, and allergies are more prone to developing eczema. However, it is essential to understand that you can still develop eczema if no one else in the family has ever had it.
Are You Born with Eczema?
One question we often get is: Are you born with eczema? The truth is, most people are not born with eczema symptoms, but they may be born with a hereditary risk that affects the immune system or skin barrier and makes one more prone to developing eczema in the first few years of their life, especially after coming in contact with triggers such as dry air, harsh soaps, rough fabrics, etc.
According to the National Eczema Association, children whose both parents have eczema are estimated to have about a 50% chance of developing eczema themselves, and having at least one parent with eczema is a known risk factor for the condition. Genetics interact with environmental factors to influence whether and when eczema appears. So while genetics are present from birth, eczema does not always appear immediately.
Can You Develop Eczema Later in Life without Family History?
The answer to “Can you develop eczema later in life?” is Yes. Even if you have never had eczema in your childhood and do not have a family history of the condition even then you can still develop it later in life.
This scenario is often known as adult-onset eczema or sudden-onset eczema. Many people claim to have eczema developing in their 30s for the first time. In these cases, the causes of eczema are usually the
- Impaired skin barrier
- Environmental triggers
At times, because of aging, hormonal changes in the body, or even due to experiencing any other skin or medical condition, the skin’s protective barrier becomes weak, which makes it hard for the barrier to retain moisture and protect the skin against outside irritants and allergens.
As a result, when your skin comes in contact with the irritants, it can trigger an eczema flare-up that leads to red, dry, itchy skin. Some common factors that trigger eczema are:
Biological Factors
- Stress and anxiety
- Asthma
- Allergies
- Chronic dry skin
- Hormonal changes
- Skin barrier dysfunction
Environmental Factors
- Hard water
- Cold, dry air
- Chemicals in skincare products
- Smoke
- Irritating fabrics
- Metal
- Poison ivy
The triggers may vary from person to person, so in order to pinpoint what your trigger is, it is best to consult a dermatologist.
How to Control Eczema Symptoms Naturally?
While there is no permanent cure for eczema, the symptoms can be effectively managed at home with proper care. Here are a few things that you must do.
Follow an Eczema Skincare Routine
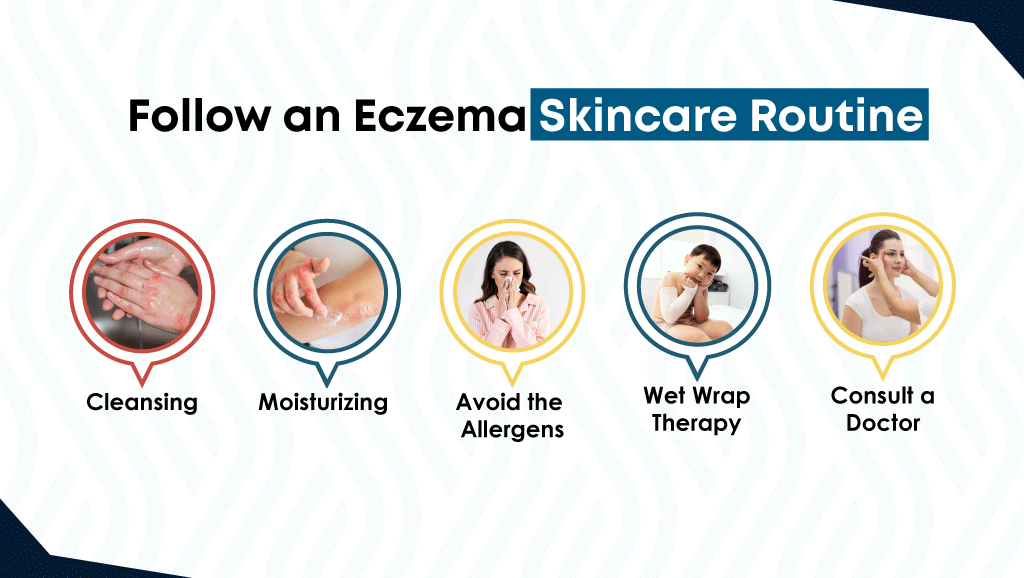
When you have eczema, the skin becomes sensitive, which makes it essential to follow a proper skincare routine and be consistent in it. Your routine should include the two following steps.
Step 1: Cleansing
- Use a fragrance-free eczema body wash to cleanse your skin at least once daily.
- Make sure to use lukewarm or cool water instead of hot water to take a bath.
- Massage the body wash onto your skin using your hands instead of a harsh scrub or loofah.
- Thoroughly rinse your skin and make sure not to leave any residue behind on the skin.
- After the bath, pat your skin dry instead of rubbing it.
Step 2: Moisturizing
- Use a hypoallergenic eczema moisturizing cream to moisturize your skin at least twice daily.
- Moisturize the skin once in the morning and once before going to bed.
- If you notice that your skin is becoming dry more often, then moisturize it after every few hours.
- Massage the cream onto your skin with your fingers in back and forth motion instead of rubbing it.
Avoid the Allergens
If you know the triggers that cause an eczema flare-up or make one worse, then try to avoid them as much as possible. This can help soothe the symptoms and prevent future flare-ups.
Wet Wrap Therapy
Wet wrap therapy can also help soothe the intense itching and irritation associated with eczema. However, this should only be done when and as advised by the doctor. In this therapy, a thick emollient prescribed by the doctor is applied to the skin, then covered with a wet gauze, followed by a dry gauze or cloth.
Consult a Doctor
If your eczema is not getting better with an eczema skincare routine or the symptoms are getting worse, then consult a doctor. The doctor may prescribe the use of certain medications such as topical steroids, antihistamines, and JAK inhibitors, along with the skincare routine, to soothe symptoms.
Manage Eczema with Dermal Defense

As we discussed before, following a proper skincare routine is essential; it is also important to use the right products as well. The harsh chemicals in skincare products can further irritate the skin and make your eczema worse.
This is why Dr. Eddie, an expert pediatrician, developed products that are safe for use on eczema-prone, sensitive skin.
Dermal Defense Fragrance-Free Body Wash gently cleanses the skin without stripping away the natural oils. It is sulfate-free, paraben-free, soap-free, and pH-balanced, which makes it safe to be used on sensitive skin.
The Dermal Defense Eczema Moisturizer helps hydrate the skin and strengthen its natural barrier. It is infused with ingredients like the licorice root extract, glycerin, and snow white petrolatum that help soothe the eczema symptoms and form a layer on the skin that strengthens the protective barrier.
Conclusion
So, is eczema genetic or hereditary? The answer is yes. Genetics can increase the risk of developing eczema. People who have a family history of eczema, asthma, hay fever, and allergies are more likely to experience it.
However, along with hereditary risk factors, there are other factors such as impaired skin barrier, overactive immune system, and environmental triggers that can also cause eczema. So even if you don’t have a family history of eczema, you can still develop it later in life.
Eczema can be easily managed at home by following a proper skincare routine, avoiding triggers, and using the medications advised by the doctor. If you are searching for eczema-friendly skin care products, then try Dermal Defense Eczema Skincare Bundle.
FAQs
- Are you born with eczema or can you develop it?
Most people are not born with visible eczema, but they may be born with a genetic predisposition that affects how their skin barrier and immune system function. This makes the skin more vulnerable to dryness, irritation, and inflammation, which can trigger eczema.
- Is eczema a birth defect?
No, eczema is not a birth defect. It is a chronic inflammatory skin condition influenced by genetics and environmental factors. While certain gene variations can increase the risk of developing eczema, the condition itself is not present at birth in most cases.
- Who is more prone to eczema?
People who are more at risk of developing eczema include:
- Individuals with a family history of eczema, asthma, hay fever, or other allergic conditions
- People with naturally dry or sensitive skin
- Those with a weakened or impaired skin barrier
- Individuals with an overactive or dysregulated immune response
- What is the best cure for eczema?
There is no permanent cure for eczema, but it can be effectively managed by avoiding known triggers and maintaining a consistent skincare routine. Your routine should include the use of an eczema body wash to cleanse the skin daily and an eczema cream to moisturize the skin twice daily.
- Eczema and Mental Health: How It Affects Anxiety & Depression - January 29, 2026
- Eczema and Genetics: Is It Hereditary? - January 29, 2026
- Is Eczema Contagious? Debunking Myths - January 27, 2026